GYNECOMASTIA
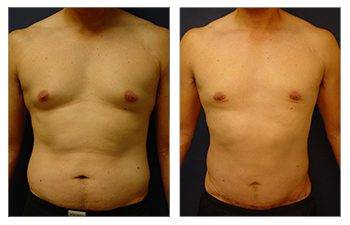
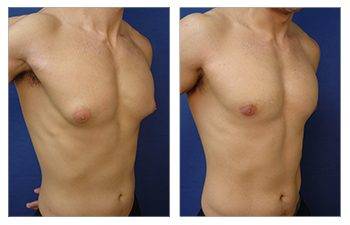
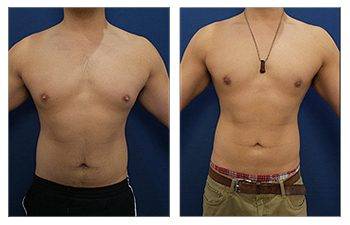
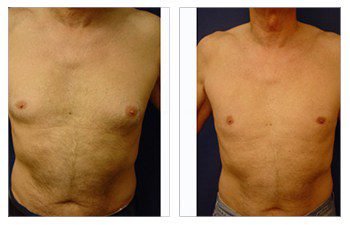
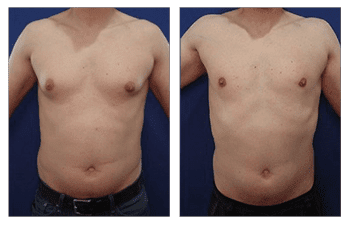
Gynecomastia CASE STUDIES
Introduction To Gynecomastia
The community regards SurgiSculpt surgeons highly for their artistry in performing gynecomastia surgery. We developed the Gynecomastia Procedure Protocol in Newport Beach to ensure that each patient attains their maximum potential following surgery. Gynecomastia in Newport Beach optimizes all aspects of your male breast surgery experience, including your initial confidential consultation, an anxiety-free operation, proprietary surgical protocols, comfortable postoperative recovery, a speedy return to full activity, and maintenance of long-term results.
Gynecomastia Surgery Consultation
During your initial gynecomastia consultation with your surgeon, you will have the opportunity to convey to him or her exactly what your concerns are. To ensure optimum results, your chest is evaluated in four independent quadrants detailing your excess breast tissue and excess skin. Assessing your chest in separate quadrants allows our surgeons to accurately assess the amount of excess fat/fibrous tissue and degree of skin redundancy to ensure optimum breast contouring results.
If the degree of fat/fibrous tissue excess and skin redundancy is minimal, you are a candidate for using traditional liposuction. If you present with minimal fat/fibrous tissue fullness and moderate skin redundancy, you should consider adding Renuvion J Plasma to tighten your skin. If the fat/fibrous tissue fullness is moderate, but the skin redundancy is minimal, you will benefit from VASER liposuction. If the fat/fibrous tissue fullness and skin redundancy are moderate, you will benefit from VASER and Renuvion J Plasma. You will benefit from direct glandular excision and liposuction when the soft tissue is extensive, and skin redundancy is minimal. If the soft tissue fullness is extensive and skin redundancy is moderate, you will benefit from direct excision, liposuction, and Renuvion J plasma. If the soft tissues and skin redundancy are extensive, you will benefit from direct excision using a wedge mastectomy.
| Soft Tissue Fullness | Skin Redundancy | Treatment |
| Minimal | Minimal | Traditional Liposuction |
| Minimal | Moderate | Traditional Liposuction and Renuvion J Plasma |
| Moderate | Minimal | VASER Liposuction |
| Moderate | Moderate | VASER Liposuction and Renuvion J Plasma |
| Extensive | Minimal | Direct Gland Excision and Traditional Liposuction |
| Extensive | Moderate | Direct Gland Excision, Liposuction, and Renuvion J Plasma |
| Extensive | Extensive | Wedge Mastectomy |
Gynecomastia Surgery Procedure
Depending on the amount of excess fat, glandular fibrous tissue, and skin excess over the breast, the patient will be tailored to a customized surgical treatment of gynecomastia. Surgery for gynecomastia options includes traditional liposuction, Renuvion J Plasma, VASER liposuction, direct gland excision, and a wedge mastectomy.
The end goal of gynecomastia treatment is to get a flattened and defeminized chest by completing a breast reduction procedure. Breast reduction surgery eliminates fullness in soft tissues and overlying skin, making the male breasts appear more feminine.
Traditional liposuction
Traditional liposuction describes the use of conventional liposuction cannulas to remove the fat. First, a numbing and constricting solution, called a tumescent solution, is infiltrated throughout the four quadrants of the breast. The four quadrants divide the breast into discreet sections labeled upper medial, lower medial, upper lateral, and lower lateral. This division of regions allows our SurgiSculpt surgeons to accurately reduce fatty tissues with specific attention to correcting any asymmetries present throughout each breast. Typical volumes of tumescent infiltration volumes include 50 to 100 per quadrant. Once the infiltration area has blanched, hollow-bore cannulas are used to remove the minimal to moderate fatty tissues and fibrous glands. The advantage of using traditional liposuction is less fluid accumulation in the postoperative recovery phase. This effective treatment means faster recovery time.
Renuvion J Plasma
Renuvion J plasma is a proprietary minimally invasive tool that can tighten moderate loose or redundancy skin over the chest area. It tightens loose or redundant skin by delivering thermal energy to connective tissue molecules called collagen. Collagen molecules are heated by an arc of energy produced from the combined energy of helium-activated plasma cells and Renuvion J plasma. This thermal energy results in a shrink-wrap effect of the collagen molecules. The net result is the shortening of collagen molecules throughout the soft tissues, and the deepest layer of the skin called the dermis. The advantage of Renuvion J plasma is that the energy can be delivered through sleek wands using the liposuction port sites already created.
VASER Liposuction
VASER liposuction possesses the advantage of ultrasound technology which helps cut through moderate fat and fibrous glandular tissues. It is advantageous to patients with a larger discoid of glandular tissue that ultrasound waves can cavitate. Cavitation describes how ultrasound waves create air bubbles in the soft tissue, which break up fat cells from solid clusters to a single-cell liquid medium and break down firm scar tissues and even glandular cells. The advantage of VASER liposuction is that it can provide definitive removal of moderate fat and fibrous tissues and scar tissue if prior liposuction has been attempted. The disadvantage is that residual liquified fatty cells may remain, necessitating lymphatic message and drainage into lymph node basins.
Direct Gland Excision
Direct Gland excision describes the cutting out of the gland using a direct approach. The gland under the nipple and areola is approached by making an incision along the lower edge of the areola. This incision is made in the shape of a smiley face and positioned along the same junction of the pink areola and lighter breast mound skin. Great care is taken to protect the skin edges using heat-protecting retractors. The epithelial component is first defined before its resection. A small amount of gland is left on the undersurface of the nipple and areola for two reasons. First, preserving a cuff of the gland under the skin will preserve blood flow to the areola. Moreover, leaving the cuff will prevent a divot deformity since it needs to smoothly transition to the breast periphery. Remember that this region must be liposuctioned. Thus the thickness of the cuff must match the thickness of soft tissue preserved in the periphery to ensure a smooth breast contour.
Wedge Mastectomy
A wedge mastectomy is reserved for extensive fat and fibrous tissues and extensive skin redundancy, making minimally invasive gynecomastia surgery alternatives ineffective. Instead, large amounts of soft tissues and skin must be excised en-block to eliminate both concerns. The excised wedge is positioned along the inframammary crease so that the final incision will be more hidden. The final consideration is whether the nipple and areola can be maintained in their position or whether the nipple and areola must be transposed to a higher, more aesthetically pleasing position. For men, the nipple and areola are positioned just above the inframammary crease and just lateral to the mid-meridian line. The preoperative nipple position and the desired final position determine whether a nipple transposition is needed.
Gynecomastia Surgery Length
Your male breast reduction surgery may take 1 to 4 hours, depending on the required procedures.
Gynecomastia Surgery Anesthesia
Your breast reduction surgery may be performed with local anesthesia, intravenous sedation called twilight anesthesia, or general anesthesia, depending on the complexity of the surgery required.
Gynecomastia Surgery Place of Treatment
Surgical treatments may be performed in an outpatient surgical facility, office-based surgical facility, or at a hospital.
Gynecomastia Surgery Side Effects
- Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. This impairment is typically temporary and resolves within a few months.
- Scarring: Incisions may be lumpy and red for a few months, but incisions become less apparent over time and can even fade to thin white lines. In general, due to improvements in suture quality, patients can expect superior results today compared to just a decade ago. It is important to acknowledge that smoking impedes the healing process and will result in more prominent surgical scars in patients who smoke.
- Breast/Nipple asymmetry: Breasts may not be the same size and shape, and nipples could be positioned unevenly depending on preoperative asymmetry. Furthermore, when liposuction is used, you may experience uneven contouring or skin redundancy that should tighten over time.
Gynecomastia Surgery Risks
- Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period, which pools into a dissected pocket. Hematomas provide a perfect medium for harboring the growth of bacteria. If the patient has an infection anywhere in the body, the bacteria will travel through the bloodstream and resettle in the hematoma, leading to infection and subsequent wound development. Drains can be placed in surgery to avoid a hematoma so any fluid accumulation can be drained. In addition, patients are evaluated preoperatively to ensure they do not have a blood clotting deficiency. Finally, patients are asked to wear a breast compression garment for the 1st two weeks to prevent hematoma formation.
- Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by the surgical elevation of the soft tissue and the disruption of vessels. This fluid may accumulate if the patient's blood count is low and the patient's nutrition is poor. When nutrition is poor, protein levels in the blood are diminished, which promotes leakage of this plasma fluid out of vessels. This fluid can be a nuisance to patients, often requiring several aspirations in the office before its resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery and effectively prevent seroma formation. Additionally, patients are asked to wear a breast compression garment over the 1st two weeks to prevent seroma formation.
- Infection: An infection can occur after gynecomastia surgery, disrupting surgical incision lines and leaving the patient with an open breast wound. Prolonged antibiotics may be required to fight infection and prevent further infection extension. The risk of infections is avoided by using the sterile technique, intra-operative antibiotics, and sealing all incision sites so bacteria can't get in through external contact. In addition, infections are less likely in patients who don't smoke cigarettes or in smokers who quit smoking for at least one month before surgery.
- Pulmonary embolism: Blood clots may form in leg veins during surgery when the patient is under general anesthesia. Patients with a leg vein clot will complain postoperatively of pain in their calves. The patient with this complaint should be taken seriously and treated if a vein clot is diagnosed. Early treatment of patients with a deep leg vein will avoid the migration of leg vein clots to the heart and lungs, causing a pulmonary embolism. Even though pulmonary emboli are rare, pulmonary emboli are the leading cause of death after surgery. Pulmonary emboli must be detected early by performing a CT Scan and should be treated urgently.
- Skin edge compromise/death: The skin incision can be disrupted if the skin edge is vascularly compromised and dies or if there is a local infection. Counseling patients best avoid this complication of the terrible consequences of nicotine in cigarettes. Nicotine will clog all the small vessels found in the skin, which are critical for delivering nutrients and healing the skin's edge. Gynecomastia surgery patients must quit smoking for at least one month before surgery. In addition, uncontrolled diabetes can lead to the undesired sloughing of the skin. Diabetic patients are urged to be vigilant about controlling their blood sugar levels before surgery. Patients who develop an open wound will require prolonged local wound care with frequent dressing changes. Unfortunately, any delays in healing the skin edges will compromise your aesthetic outcome.
Gynecomastia Surgery Recovery
Most Patients can return to work and resume normal activities 7 to 10 days after surgical treatment. Physical activity may be initiated within two weeks following surgery. Strenuous activities such as heavy lifting can usually be performed four weeks after surgery. Any residual contour irregularities should be resolved within three months following the treatment of gynecomastia. These recovery times may be altered by the degree of gynecomastia, and the treatment for gynecomastia recommended.
Surgical procedures such as liposuction alone will have shorter recovery than, for example, a wedge mastectomy requiring skin resection. Eliminating excess skin, especially in dark skin individuals, may require a longer recovery period to allow incision lines to fade. Your body mass index and the degree of invasive technique advocated will affect full recovery.
Gynecomastia Surgery Duration of Results
Breast reduction in men usually yields permanent results unless patients experience significant weight gain or continue the consumption of causative agents. Identified causative agents are numerous and have included consumption of alcohol, marijuana, and chronically prescribed steroids.
GYNECOMASTIA FREQUENTLY ASKED QUESTIONS
Am I a good candidate for gynecomastia surgery (male breast surgery)?
You should only consider gynecomastia surgery if you are in good general health and have matured physically and emotionally. Men with firm, elastic skin will achieve the best results from male breast surgery and require less extensive surgical measures. Male breast surgery is recommended for patients who feel dissatisfied with their breast size and shape following the completion of breast development. Patients seeking surgical correction of their breast appearance should consider clinical evaluation for the cause of their breast enlargement. Clinical evaluation is important as it can unveil more serious physiological disorders and prevent a recurrence. Patients who consume large amounts of alcohol and are prescribed steroids or smoke marijuana must be counseled against the risk of reoccurrence.
What does male gynecomastia surgery (male breast surgery) involve?
Depending on the amount of excess fat, glandular tissue, and skin that a patient has, liposuction, direct excision, or both may be necessary. For patients with minimal sagging skin and minimal glandular tissue but excess fat, liposuction only may be sufficient. With liposuction, a small incision less than ½ a cm in length is created at the edge of the areola to insert a thin, hollow tube that breaks down and removes excess fat. However, most patients present with excess glandular tissue underlying the nipple-areola, which then requires an extension of the infra areolar liposuction injection site to approximately a 1-inch incision to remove the excess glandular tissue in addition to liposuction of the excess fat. In severe cases of skin redundancy and male breast sagging, direct excision of redundant skin and excess fat is required to avoid a deflated and overly sagging breast that would result from liposuction alone. In these cases, surgical incisions are placed strategically to allow for final surgical incisions in the shape of a “male breastplate,” often seen in steel armor photos. In these cases, it is also necessary to remove and resize the nipple-areola complex before replacing them in a natural and youthful position with skin grafting techniques.
How do I plan my gynecomastia surgery (male breast surgery)?
On your initial visit, your surgeon will evaluate your health status by obtaining blood work and encourage you to seek consultation with your primary care or endocrinology physician to consider a clinical workup for the cause of your enlarged breasts. Your surgeon may examine you to rule out obvious medical causes of breast enlargement, such as impaired liver function, use of estrogen-containing drugs or steroids, or obesity. Your surgery may be postponed if your breasts are enlarged due to a medical conditions.
If you are 40 years or older, have had a personal or family history of breast symptoms (tenderness, lumps, nipple discharge), or contain suspicious lesions following your breast examination, you will be asked to obtain a mammogram. The mammogram will rule out breast cancer and let your surgeon know what kind of breast composition needs to be treated, which will dictate the surgical techniques required for your surgery. If you are a smoker, you should quit for one month before breast reduction surgery to minimize skin tissue compromise. In addition, it is prudent to quit smoking for six weeks following surgery to ensure well-healed surgical incision lines. Finally, you will need to arrange for a friend or a spouse to care for any small children who may need to be lifted since you will be sore for the first couple of days following surgery.
How do I prepare for gynecomastia surgery (male breast surgery)?
Since your surgery may require general anesthesia, you must take several precautions before surgery. First, you must avoid eating and drinking after midnight on the day before surgery. This precaution ensures that your stomach is clear of digested foods that could potentially be aspirated into your lungs during induction of anesthesia. Since you will have anesthetic medications administered throughout the case, you will remain groggy for several hours and require a ride to and from the surgery center. You should choose a conscientious caretaker who can spend the first night with you.
Where will my gynecomastia surgery (male breast surgery) be performed?
Depending on the method of breast reduction and type of anesthesia, gynecomastia surgery can be performed at a hospital, outpatient surgical facility, or office-based surgical facility. If general anesthesia is required, the surgery must be performed in an operating room that is part of a hospital institution or an outpatient surgery center. Patients operated on at an office-based operating room must verify that the office facility is accredited by a surgical accreditation body such as AAAASF.
What type of anesthesia will be used for my gynecomastia surgery (male breast surgery)?
Depending on the complexity of your surgery, your surgeon will recommend intravenous sedation in combination with local anesthesia or general anesthesia. Your plastic surgeon will discuss the type of sedation you will require with you during the consultation for gynecomastia surgery.
What should I expect after gynecomastia surgery (male breast surgery)?
Regardless of the surgical technique, patients will experience bruising, swelling, and discomfort for the first few days after surgery. Your physician will prescribe pain medication and antibiotics to address these problems. After surgery, you must wear an elastic pressure garment for 1 to 2 weeks at all times and for two more weeks only at night. Stitches are all internal, and external tapes remain in place for one month. Generalized swelling will resolve over the first month. Strenuous activities such as heavy lifting should be avoided for about four weeks, but patients can usually return to work and resume light activities within 7 to 10 days after surgery.
What results can I expect after gynecomastia surgery (male breast surgery)?
Breast reduction in men usually yields permanent results unless patients experience significant weight gain or continue consumption of causative agents. You should expect permanent surgical scarring, but your surgeon will try to conceal the scars in the breast's natural contours. By providing a thorough preoperative workup, a safe intraoperative course, and frequent postoperative visits, patients should expect a speedy recovery and return to a more aesthetically pleasing physique and a more comfortable lifestyle. Men who undergo gynecomastia surgery are extremely satisfied with their flattened and better-contoured chests and gain immense self-confidence after surgery.
When will I be able to return to work following gynecomastia surgery (male breast surgery)?
Patients can usually return to work in 7 to 10 days if their job does not include heavy physical stress. Patients with more strenuous jobs will require four weeks before returning to work.
Are there any side effects associated with gynecomastia surgery (male breast surgery)?
a) Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. This impairment is typically temporary and resolves within a few months.
b) Scarring: Incisions may be lumpy and red for a few months, but incisions become less apparent over time and can even fade to thin white lines. In general, due to improvements in suture quality, patients can expect superior results today compared to just a decade ago. It is important to acknowledge that smoking impedes the healing process and will result in more prominent surgical scars in patients who smoke.
c) Breast/Nipple asymmetry: Breasts may not be the same size and shape, and nipples could be positioned unevenly depending on the degree of preoperative asymmetry. Furthermore, when liposuction is used, you may experience uneven contouring or skin redundancy that should tighten over time.
Are there any risks associated with gynecomastia surgery (male breast surgery)?
a) Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period, which pools into a dissected pocket. Hematomas provide a perfect medium for harboring the growth of bacteria. If the patient has an infection anywhere in the body, the bacteria will travel through the bloodstream and resettle in the hematoma, leading to infection and subsequent wound development. Drains can be placed in surgery to avoid a hematoma so any fluid accumulation can be drained. In addition, patients are evaluated preoperatively to ensure they do not have a blood clotting deficiency. Finally, patients are asked to wear a breast compression garment for the 1st two weeks to prevent hematoma formation.
b) Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by the surgical elevation of the soft tissue and the disruption of vessels. This fluid may accumulate if the patient's blood count is low and the patient's nutrition is poor. When nutrition is poor, protein levels in the blood are diminished, which promotes leakage of this plasma fluid out of vessels. This fluid can be a nuisance to patients, often requiring several aspirations in the office before its resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery and effectively prevent seroma formation. Additionally, patients are asked to wear a breast compression garment over the 1st two weeks to prevent seroma formation.
c) Infection: An infection can occur after gynecomastia surgery, disrupting surgical incision lines and leaving the patient with an open breast wound. Prolonged antibiotics may be required to fight infection and prevent further infection extension. The risk of infections is avoided by using a sterile technique, intra-operative antibiotics, and sealing all incision sites so that bacteria can't get in through external contact. In addition, infections are less likely in patients who don't smoke cigarettes or in smokers who quit smoking for at least one month before surgery.
d) Pulmonary embolism: Blood clots may form in leg veins during surgery when the patient is under general anesthesia. Patients with a leg vein clot will complain postoperatively of pain in their calves. Patient's with this complaint should be taken seriously and treated if a vein clot is diagnosed. Early treatment of patients with a deep leg vein will avoid migrating leg vein clots to the heart and lungs, causing pulmonary embolism. Even though pulmonary emboli are rare, pulmonary emboli are the leading cause of death after surgery. Pulmonary emboli must be detected early by performing a CT Scan and should be treated urgently.
e) Skin edge compromise/death: The skin incision can be disrupted if the skin edge is vascularly compromised and dies or if there is a local infection. Counseling patients best avoid this complication on the terrible consequences of nicotine in cigarettes. Nicotine will clog all the small vessels found in the skin, which are critical for delivering nutrients and healing the skin's edge. Male breast surgery patients are usually mandated to quit smoking for at least one month before surgery. In addition, uncontrolled diabetes can lead to the undesired sloughing of the skin. Diabetic patients are urged to be vigilant about controlling their blood sugar levels before surgery. Patients who develop an open wound will require prolonged local wound care with frequent dressing changes. Unfortunately, any delays in healing the skin edges will compromise your aesthetic outcome.
GYNECOMASTIA SURGERY PATIENT-SPECIFIC QUESTIONS
What is gynecomastia?
Gynecomastia is a condition in males where the breasts become enlarged and appear “female-like.” Patients with gynecomastia may have excess fat, glandular tissue, and a variable degree of redundant skin tissue.
What causes enlarged breasts in men?
The causes of enlarged breasts in men are several. They include genetic predisposition or disorders, natural aging changes, puberty, obesity, steroid abuse, chronic liver disease, side effects of estrogen-containing medications, excessive drinking, drug abuse such as marijuana use, or certain brain or breast tumors. Enlarged breasts can be common in adolescent boys and are usually only temporary. Interestingly, enlargement of breasts may affect only one and not both breasts.
It is important to determine the cause of enlarged breasts before gynecomastia surgery to address any pertinent medical problems and discontinue any activities that may preclude you from the recurrence of enlarged breasts. In rare cases, surgery may not be indicated.
Are enlarged breasts in men a dangerous condition?
Typically, enlarged breasts are not dangerous to a patient's health. Although extremely rare, breast cancer may be a cause of enlarged breasts. Breast cancer should be considered when there is enlargement in only one breast because gynecomastia usually occurs in both breasts. When there is a concern about breast cancer, patients must get a mammogram before surgery. Additionally, patients may harbor a brain tumor resulting in increased estrogen production, which requires diagnosis and treatment before considering any breast surgery.
How common is gynecomastia?
Some studies have estimated that 60-70% of males have gynecomastia. This condition is particularly common in newborns, adolescents, and older men. Males from these age groups have an exceptionally high frequency of gynecomastia due to drastic hormone fluctuations. An abnormal ratio of estrogens to testosterone in the body affects tissue growth in the breast region.
Will I need liposuction or excision of breast tissue during gynecomastia surgery?
The technique of gynecomastia surgery that you will require depends on the degree of redundant breast fat, glandular tissue, and skin. Patients with firm skin, minimal glandular tissue, and excess fat may require liposuction only. However, most patients do present with excess glandular tissue. Thus, they will require a combination of liposuction and direct excision of the glandular tissue underlying the nipple and areola complex. Less often, patients with extensive redundant skin and sagging breasts may require direct excision of the breast skin, fat, and glandular tissue. The nipple-areola complex must be replaced in these patients as a skin graft.
Will there be any scarring?
When liposuction and direct excision of the glandular tissue are required, surgical incisions are limited, and scarring is not typically a concern. In contrast, when direct excision of the breast skin, fat, and glandular tissue is required, patients must be counseled about the surgical scars that will ensue. These scars are placed appropriately to mimic an “armor plate,” and surgical incisions are repaired using a meticulous technique. Although these scars typically remain red for a few months, they will eventually fade into thin white lines.
Will my insurance cover male breast surgery?
Since gynecomastia is usually not detrimental to a patient's physical health, gynecomastia surgery is typically not covered by insurance companies. However, coverage policies may vary, and in rare cases, when it is documented that the enlarged breasts have resulted in psychological trauma to the patient, your plastic surgeon will help determine if insurance coverage is attainable.
HOW OUR PATIENTS FEEL ABOUT US:
Refresher
I came to the office for botox and Juvederm with my best friend. The Dr was very knowledgeable and made me feel comfortable. Both procedures were pain free and the results were amazing and subtle. I have been getting lots of compliments about how refreshed I look. Will definitely be recommending him to all my friends!!
Breast Reconstruction Following Mastectomy
I've had several procedures with SurgiSculpt following my mastectomy. The entire staff is great, especially both massage therapists (Theresa and Polly) as well as James. I am going to do nipple tattooing with them as well and then I will finally be all done! I couldn't be happier to have found themand close this chapter of my life.
Awesome experience
Awesome experience! The doctor knew exactly what I wanted and everything I asked for was perfect! Easy to work with, great results. With this type of procedure you need a good listener, What a great listener.