BREAST RECONSTRUCTION
breast reconstruction revision Surgery CASE STUDIES
Introduction to Breast Reconstruction
The art of Breast Reconstruction has undergone several advancements over the last decade resulting in superior breast reconstruction outcomes.
Two important advancements in Reconstructive Breast Surgery have included:
- The advent of superior implant availability
- Biologic skin substitutes.
First, current implant selection has expanded as there are far more implant shapes and sizes available (varied by base width and height projection). This expanded selection of implants allows the surgeon to better match the reconstructed breast to the patient’s original breast shape. The introduction of “gummy bear” implants, implants that are firmer and less prone to wrinkling, has reduced the risk of rippling, or wrinkling of the breast skin; rippling is a term describing contour irregularities frequently observed due to thinning of the breast skin following mastectomies. Second, the use of biologic skin substitutes created from human donors allows the surgeon several advantages not previously available; these include complete coverage of the implant without compromising lower pole fullness and recreation of the inframammary crease (the natural junction between the breast and abdomen) which is violated during the mastectomy. A final advancement in breast reconstruction includes the use of fat grafting which allows for fine-tuning of breast mound shape.
Although implants provide replacement of the breast mound proper, subtle skin contour irregularities may be created during mastectomy and persist following reconstruction. These subtle skin irregularities can now be corrected with the use of fat material harvested from any area of your choice and molded into your breast skin to optimally smoothen your breast skin contour. Newport Beach, Orange County Plastic Surgeon SurgiSculpt is well regarded for his artistry and reconstructive breast surgery outcomes taking advantage of the above recent advances.
Breast Reconstruction Procedure
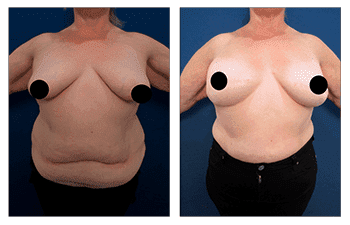
Restoration of normal breast size, shape, and appearance after removal of one, part of one, or both breasts. Restoration of breasts can be accomplished by two methods and include: a)use of silicone breast implant that is covered and protected by muscle, fat and skin accompanied or human-like synthetic tissue (alloderm versus HD-flex) following expansion of the overlying and remaining breast skin tissue by use of a breast expander, or b)a tissue flap procedure which utilizes a woman’s own muscle, fat and skin from her tummy, back, thighs, or buttocks to create a breast mound. Following reconstruction of desired breast mound and shape, patients undergo nipple-areola reconstruction by local tissue arrangement and skin grafting. Finally, patients who complete unilateral breast reconstruction usually choose to undergo contralateral breast symmetry procedures involving a lift procedure and implant placement.
Breast Reconstruction Length
1 to 6 hours depending on the surgical method and stage.
Breast Reconstruction Anesthesia
General anesthesia.
Breast Reconstruction Place of Treatment
Outpatient surgical suite or hospital operating room.
Breast Reconstruction Side Effects
a) Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. Tissue flap surgery includes the risk of partial or complete loss of the flap and a loss of sensation at both the donor and reconstructed site. This impairment is typically temporary and resolves within a few months. In rare cases, the loss of feeling can last longer or become permanent due to damage to sensory nerves that are too small to detect by direct vision during surgery.
b) Scarring: Incisions may be lumpy and red for a few months, but incisions become less apparent over time and can even fade to thin white lines. Healing scars can usually be covered by a bra or swimsuit top. It is important to acknowledge that smoking impedes the healing process and will result in more prominent surgical scars.
c) Breast/Nipple asymmetry: Breasts may not be the same size and shape and nipples could be positioned unevenly depending on the degree of preoperative asymmetry and depending on whether a contralateral breast symmetry procedure has been performed.
Breast Reconstruction Risks
a) Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period which pools into a dissected pocket. Hematomas provide a perfect medium for harboring the growth of bacteria. In fact, if the patient has an infection anywhere in the body, the bacteria will travel through the bloodstream and resettle in the hematoma; this can lead to an infection and subsequent wound development. In order to avoid a hematoma, drains can be placed in surgery so that any fluid accumulation can be drained. Drains are usually kept in place for 1 to 2 weeks. In addition, patients are evaluated preoperatively to make sure that they do not have a blood clotting deficiency.
b) Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by the surgical elevation of the soft tissue and disruption of vessels. This fluid may accumulate if the patient’s blood count is low and/or the patient’s nutrition poor. When nutrition is poor, protein levels in the blood are diminished which promotes leakage of this fluid out of vessels. This fluid can be a nuisance to patients often requiring several aspirations in the office prior to its resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery and are very effective in preventing seroma formation.
c) Infection: An infection can occur after breast reconstruction surgery especially when expander implant reconstruction is used. An infection may result in disruption of surgical incision lines and may leave the patient with an open breast wound. When implant expander reconstruction is performed an infected implant may be extruded. Prolonged antibiotics and possible removal of antibiotics may be required to fight infection and to prevent further extension of the infection. The risk of infections is avoided by using the sterile technique, using intra-operative antibiotics, and sealing all incisions sites so that bacteria can’t get in through external contact. In addition, infections are less likely in patients who don’t smoke cigarettes or in smokers who quit smoking for at least 1 month prior to surgery. If an infection occurs and the implant has been removed, the patient’s reconstruction will be delayed by at least 3 months.
d) Pulmonary embolism: Blood clots may form in leg veins during any surgery when the patient is under general anesthesia. Patients with malignancy such as in patients with breast cancer have a higher risk of clot formation. Patients with a leg vein clot will complain postoperatively of pain in their calves. The patient with this complaint should be taken seriously and treated if a vein clot is diagnosed. Early treatment of patients with a deep leg vein will avoid migration of leg vein clots to the heart and lungs causing a pulmonary embolism. Even though pulmonary emboli are rare, pulmonary emboli are the leading cause of death after surgery. Pulmonary emboli must be detected early by performing a CT Scan and should be treated urgently.
e) Tissue death (necrosis): Following mastectomy, portions of the breast tissue may become compromised due to overly thinning of the breast skin flaps created during the mastectomy. In addition, when tissue flap reconstruction is utilized, it no uncommon to lose a portion of the transferred fat and skin. This complication will result in secondary procedures which will require debridement of compromised tissues and revision of surgical incision lines.
f) Capsular contracture: Capsular contracture causes the breast to feel hard and is caused by the hardening of a scar around a foreign body such as a breast implant. Although this scar formation is expected and a natural process that occurs when expander implant reconstruction is utilized, when the scar is overly thickened and hardened it results in breast hardening and is characterized as capsular contracture. Patients who develop capsular contracture will require further surgery to either release the scar or to remove the scar entirely.
Breast Reconstruction Recovery
Patients can usually resume normal activity around 2 weeks following expander implant reconstruction and 4 to 6 weeks following tissue flap reconstruction. In general, patients should refrain from strenuous physical activity such as heavy lifting, pulling, and pushing over the first 4 weeks following surgery. Less recovery time is required following each subsequent surgery following the initial surgery.
Breast Reconstruction Duration of Results:
Breast reconstruction results can be expected to last a lifetime. However, patients may have significant physiological changes such as excessive weight gain or loss of following pregnancy which will result in breast contour changes. In addition, the patient may require long term revision surgery following unilateral breast reconstruction since bilateral breasts will have different compositions of native breast tissue to implant ratio and will thus be affected by gravity variably. Finally, when breast implants are used, there is a risk of capsular contracture which will require further surgery.
Breast Reconstruction Frequently Asked Questions:
During the 20th century, the women’s movement drew greater attention to female problems creating a demand for breast reconstruction surgery. Furthermore, the development of safer breast implants and refined tissue flap procedures have made breast reconstruction surgery a viable option for women who suffer from the consequences of breast cancer therapy requiring breast tissue removal. The American Society of Plastic Surgeons reported that about 62,000 women underwent breast reconstruction surgery in 2004.
Breast reconstruction surgery is usually performed on patients who have had their breast removed due to cancer. Suitable patients must be in good general health and be emotionally prepared to undergo reconstructive surgery. In some cases, patients may have breast reconstruction performed at the same time that the breast is remove in order to avoid emotional stress caused by a dramatic change in physical appearance. However, patients who need radiation therapy to the underarm or chest area should wait until the cancer is entirely eliminated to undergo reconstruction surgery. Furthermore, patients may not want to deal with additional surgery during the time of breast cancer removal. You should keep in mind that breast reconstruction surgery requires significant commitment and may entail several weeks to months of office visits and multiple surgeries. Since breast reconstruction surgery can be performed at the time of breast tissue removal or at a later date, you have a lot of flexibility in determining if and when you would like to get this procedure done.
There are two methods available for breast reconstruction surgery and they involve: breast expander/implant or tissue flap reconstruction:
a) Implant reconstruction: Implant reconstruction involves replacement of the breast tissue removed with a silicone gell implant. Depending on the amount of skin removed, patients usually require a staged reconstruction utilizing an expander implant to expand the breast skin prior to placement of the final silicone implant. In addition, depending on the amount of inferior breast tissue removed which may violate the inferior breast crease (inframammary crease), patients may require a dermal matrix (created to mimic the deep, tough portion of skin) to recreate this crease. Following placement of the expander and dermal matrix, patients are serially inflated during in office procedure every two weeks until the skin is expanded adequately to tolerate the placement of the desired implant replacement. When patients are expanded to the appropriate volume, patients must wait another month prior to expander removal and final silicone implant placement. During the implant replacement procedure, most patients elect to undergo a contralateral symmetry procedure of the normal breast which involves a breast lift and implant placement. Approximately, three months following this surgery patients then undergo a final nipple areola reconstruction.
b) Flap reconstruction: Flap reconstruction typically requires the use of tissue from the back or stomach to replace the tissue lost during the breast tissue removal. In some cases, when inadequate back or stomach tissue is present, patients may require a silicone implant supplementation of their tissue flap reconstruction in order to appropriately complete their reconstruction. When utilizing tissue flap reconstruction, patients forego the expander phase as adequate skin tissue will be provided by the flap tissue. In rare cases, the tissue flap must be detached from their blood supply and reattached to breast tissue vessels by microvascular surgical technique. Reconnecting these blood vessels requires the use of a microscope and more extensive surgery. Approximately three months following this surgery, patients may complete their nipple areola reconstruction and contralateral breast symmetry procedure thus completing their reconstruction.
Because patients feel differently about the timing and method of breast reconstruction surgery, you should discuss reconstructive treatment options with a board certified plastic surgeon. During your consultation, your surgeon will evaluate your health status by obtaining blood work and check your heart with an EKG (for patients older than 40 years of age). If you are performing your reconstruction at a lateral date (delayed fashion), then you will have to obtain a mammography to verify that your treated breast is still in remission and to confirm that you do not have cancer in your contralateral breast. If you are a smoker, you should quit for 1 month prior to your breast augmentation surgery to minimize the risks of implant infection. In addition, it is prudent to quit smoking for 6 weeks following surgery to ensure a well-healed surgical incision line.
Since your surgery will require general anesthesia, you must take several precautions prior to surgery. First, you will have to avoid eating and drinking after midnight on the day before surgery. This precaution ensures that your stomach is clear of digested foods that could potentially be aspirated into your lungs during induction of anesthesia. Since, you will have anesthetic medications administered throughout the case, you will remain groggy for several hours. You may remain in the hospital overnight and will require a ride to and from the hospital. You should also choose a caretaker who is conscientious to take care of you at least the first night you return home.
After breast reconstruction surgery, you will regain your breast mound and notice that your breasts appear balanced when you are wearing a bra. However, you should expect to see differences in size, shape and feel between the reconstructed breast and your natural breast. Most women are very satisfied with their improved body image if they enter the reconstruction process with realistic expectations. Patients may also be pleased of improvements of their contralateral breast sagging.
Breast reconstruction surgeries are usually performed at a hospital operating room or an outpatient surgical suite. Follow-up and staged reconstruction procedures, such as nipple and areola reconstruction, are also performed at a hospital or an outpatient surgical facility as well.
All reconstructive breast surgeries will require general anesthesia.
Depending of the method of breast reconstruction surgery that is performed, you may remain in the hospital overnight or for a few days. When undergoing tissue flap or expander reconstruction you will have drainage tubes put in place to eliminate excess fluid from the breast pocket dissected. You may feel tired and sore for about 1 week after surgery but pain is well managed with pain medication. Most women are able to resume normal activity within 2 weeks, but it is extremely important for patients to avoid strenuous activity such as heavy lifting (more than 5 lbs.) during the recovery period for up to 4 weeks. Although sensation will return to your breast and nipple area, you should not expect the reconstructed breast to have the same feeling as a natural breast.
Most patients are able to return to work between 2 to 4 weeks following breast reconstruction surgery. Patients with jobs that require strenuous physical activity will require 4 weeks of recovery period. The recovery period is longest following the first reconstructive operation and less recovery time is needed for subsequent surgeries. Depending on the method of reconstruction used(expander implant versus tissue flap), recovery periods will vary. Patients who use breast expander/implant reconstruction will have a shorter recovery period than patients who choose to have a tissue flap procedure performed.
a) Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. However, prolonged numbness is routine following complete removal of breast tissue to treat breast cancer. Tissue flap reconstruction also results in loss of normal sensation by virtue of the nerves being disconnected when transferring tissue from the back or stomach.
b) Scarring: Incisions may be lumpy and red for a few months, but incisions become less apparent over time and can even fade to thin white lines. Healing scars can usually be covered by a bra or swim suit top. Smokers are urged to stop smoking since smoking impedes the healing process and will result in more prominent surgical scars.
c) Breast/Nipple asymmetry: Breasts may not be the same size and shape and nipples could be positioned unevenly depending on the degree of preoperative asymmetry and depending on whether a contralateral breast symmetry procedure has been performed. In addition, patients must recognize that long term aging of breasts will likely result in residual asymmetry as the reconstructed breast and contralateral normal breast tissue are comprised of different tissue to implant proportion and will age differently by the effects of gravity.
a) Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period which pools into a dissected pocket. Hematomas provide a perfect medium for harboring growth of bacteria. In fact, if the patient has an infection anywhere in the body, the bacteria will travel through the blood stream and resettle in the hematoma; this can lead to an infection and subsequent wound development. In order to avoid a hematoma, drains can be placed in surgery so that any fluid accumulation can be drained. Drains are usually kept in place for 1 to 2 weeks. In addition, patients are evaluated preoperatively to make sure that they do not have a blood clotting deficiency.
b) Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by surgical elevation of the soft tissue and disruption of vessels. This fluid may accumulate if the patient’s blood count is low and/or the patient’s nutrition poor. When nutrition is poor, protein levels in the blood are diminished which promotes leakage of this fluid out of vessels. This fluid can be a nuisance to patients often requiring several aspirations in the office prior to its resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery and are very effective in preventing seroma formation.
c) Infection: An infection can occur after breast reconstruction surgery especially when expander implant reconstruction is used. An infection may result in disruption of surgical incision lines and may leave the patient with an open breast wound. When implant expander reconstruction is performed an infected implant may be extruded. Prolonged antibiotics and possible removal of antibiotics may be required to fight an infection and to prevent further extension of the infection. Risk of infections are avoided by using sterile technique, using intra-operative antibiotics, and sealing all incisions sites so that bacteria can’t get in through external contact. In addition, infections are less likely in patients who don’t smoke cigarettes or in smokers who quit smoking for at least 1 month prior to surgery. If an infection occurs and the implant has be removed, the patient’s reconstruction will be delayed by at least 3 months.
d) Pulmonary embolism: Blood clots may form in leg veins during any surgery when the patient is under general anesthesia. Patient’s with a malignancy such as in patients with breast cancer have a higher risk of clot formation. Patients with a leg vein clot will complain postoperatively of pain in their calves. Patient’s with this complaint should be taken seriously and treated if a vein clot is diagnosed. Early treatment of patients with a deep leg vein will avoid migration of leg vein clot to the heart and lungs causing pulmonary embolism. Even though pulmonary emboli are rare, pulmonary emboli are the leading cause of death after surgery. Pulmonary emboli must be detected early by performing a CT Scan and should be treated urgently.
e) Tissue death (necrosis): Following breast tissue removal (mastectomy), portions of the breast tissue may become compromised due to overly thinning of the breast skin flaps created during the mastectomy. In addition, when tissue flap reconstruction is utilized, it is not uncommon to lose a portion of the transferred fat and skin. This complication will result in secondary procedures which will require debridement of compromised tissues and revision of surgical incision lines.
f) Capsular contracture: Capsular contracture causes the breast to feel hard and is caused by hardening of a scar around a foreign body such as a breast implant. Although this scar formation is expected and a natural process that occurs when expander implant reconstruction is utilized, when the scar is overly thickened and hardened it results in breast hardening and is characterized as capsular contracture. Patients who develop capsular contracture will require further surgery to either release the scar or to remove the scar entirely.
Breast Reconstruction Patient-Specific Questions:
Breast reconstruction surgery involves the creation of a new breast to replace one that has been surgically removed, usually due to breast cancer treatment. A plastic surgeon will rebuild the breast so that it is similar in size, shape and feel to the original breast.
Breast implantation should not interfere with the results of mammograms. However, it is suggested that patients go to an imaging center with technicians that are experienced in obtaining accurate mammogram results from patients who have breast implants.
Yes, many women prepare for breast reconstruction surgery at the same time as breast removal. This has the advantage of avoiding the emotional trauma of viewing an absent breast and could also eliminate the need for a staged tissue expansion and breast implant reconstruction.
Since implant reconstruction is a less extensive procedure, it is usually recommended for older patients or very thin women who may not have sufficient tissue over their stomachs or back for tissue flap reconstruction. Expander/implant reconstruction requires shorter operative times and subsequently shorter recovery period compared to tissue flap reconstruction because the former is less invasive. Furthermore, expander/implant reconstruction allows plastic surgeons to achieve greater breast symmetry for patients who develop bilateral breast cancer surgery and/or for those who require bilateral breast reconstruction.
Tissue flap reconstruction is a complex surgery requiring prolonged operative times; therefore, this surgery is not suitable for patients with multiple medical problems. Tissue flap reconstruction is more suitable for women undergoing unilateral breast reconstruction because it uses a women’s own tissue to reconstruct a breast that better matches a naturally sagging opposite breast. Additionally, tissue flap reconstruction does not have the risks associated with breast reconstruction such as capsular contracture. Ultimately, you should discuss your treatment options with a board certified plastic surgeon before your decision.
To date, no studies have indicated that breast reconstruction causes the return of breast cancer. Additionally, breast reconstruction has not been associated in delays of detecting breast cancer recurrence.
Usually patients undergoing immediate breast reconstruction can undergo radiation treatment and chemotherapy. Patients who are expected to undergo postoperative radiation therapy are encouraged to undergo delayed breast reconstruction in order to avoid the effects of radiation on the attempted reconstruction. Patients are not encouraged to delay breast reconstruction for patients needing reconstructive surgery. Patients should verify the compatibility of reconstructive surgery and cancer treatment options with their oncologist and plastic surgeon in order to coordinate an effective treatment plan.
Breast reconstruction is always covered by medical insurance companies. In fact, follow-up surgeries, including revision surgeries, symmetry procedures of the opposite breast, and nipple areola reconstruction are all covered by insurance companies.
Follow-up procedures can be performed to balance the size and shape of the reconstructed and opposite natural breast. Revision of the reconstructed breast often requires a combination of liposuction and fat grafting employed to correct residual contour deformities. Symmetry procedures of the opposite natural breast may also require revisions to optimize contour symmetry and nipple areola malposition. Although follow-up procedures are performed, patients should also have realistic expectations about the outcome of their reconstructive surgery.