Gynecomastia stages can be a challenging concept to grasp.
This condition, impacting male breast tissue, isn’t just a uniform diagnosis. It’s far more complex than that. The key lies in understanding these stages and their implications on treatment plans. Realizing the significance of this subject matter is vital for those managing gynecomastia. Differentiating between the various Gynecomastia stages, from Grade I to IV, allows us to determine appropriate intervention strategies tailored specifically for each case.
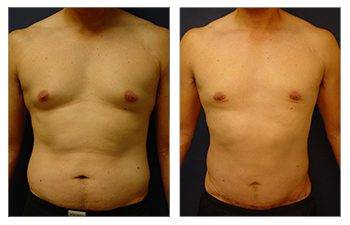
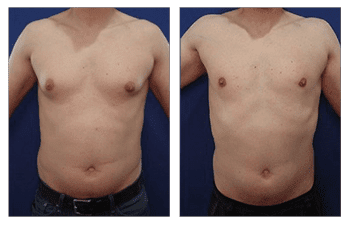
The gynecomastia stage should dictate gynecomastia surgery. The gynecomastia-treated chest should demonstrate resolution of the swollen breast appearance characteristic of a feminized breast. Gynecomastia affects both younger and older men, and thus, comprehensive analysis is crucial to determining the ideal gynecomastia treatment. Request an appointment today to complete your personalized cosmetic surgery evaluation, which will determine your surgical treatment based on the components of your extra tissue.
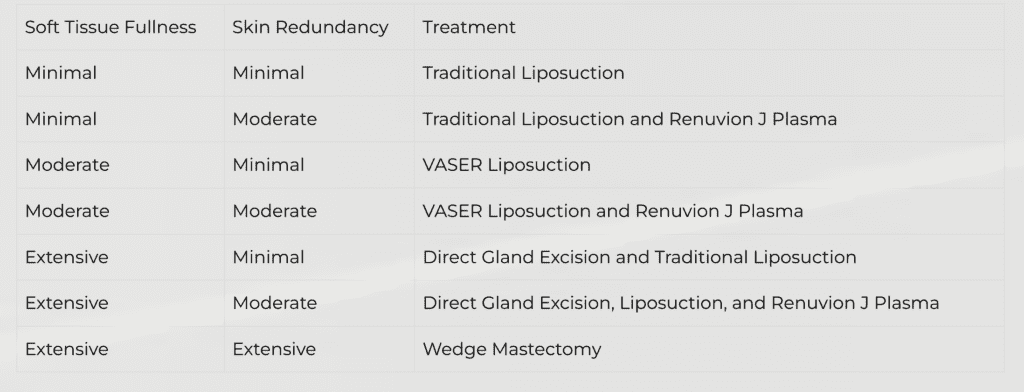
The first step is determining how much fat and gland areas are causing swollen breasts. Removal of both tissue types is critical to achieving success. A final component that affects breast grade and the gyno stages includes the degree of skin excess and resultant breast sag. Key points to treat gynecomastia are appropriate screening to determine a customized surgical plan to eliminate excess breast gland, appropriately reduce excess chest fat, and ensure optimum nipple and areola placement.
Understanding Gynecomastia Stages
Gynecomastia, a common breast condition in males, occurs due to abnormal tissue growth around the nipple area. It’s not just the physical discomfort we’re discussing here – this bilateral occurrence can also have a significant emotional impact.
Demystifying Gynecomastia
Gynecomastia should not be underestimated, as it is a non-cancerous enlargement of male breast tissue that can cause distress. Why? Gynecomastia, a non-cancerous enlargement of male breast tissue, can be an emotionally challenging experience for those it affects.
This condition arises from an imbalance between estrogen (female hormones) and testosterone (male hormones). While estrogen fuels breast tissue growth, testosterone is a brake on this process.
If we address gynecomastia through surgery, understanding its stages is crucial. The surgical plan varies significantly depending on whether you’re dealing with Grade I or Grade IV gynecomastia – yes, there are four grades.
The Four Grades of Gynecomastia:
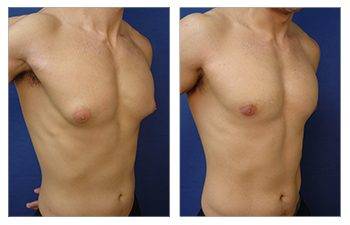
- Grade I – small enlargement without skin excess; moving onto
- Grade II, moderate enlargement without extra skin occurs;
- Grade III – moderate enlargement with minor skin excess. And finally,
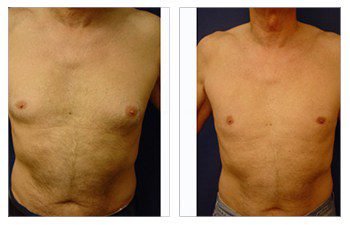
- Grade IV – marked enlargement with substantial skin redundancy, earning it the nickname “feminine breasts.” Each grade progression signifies escalating severity.
This grading system plays a crucial role in determining the best approach for corrective surgery.
Now, let’s shift gears and explore the potential psychological impact this medical issue can have on individuals.
Understanding the Psychological Impact of Gynecomastia
Gynecomastia’s psychological impact can be as profound as its physical effects. This condition, characterized by male breast enlargement, often leads to various emotional challenges, including anxiety and psychosocial discomfort.
Anxiety is a common reaction for those grappling with gynecomastia. The societal expectation for men to have flat chests amplifies this feeling. It’s common for these individuals to avoid social scenarios where their chest might be exposed, such as at the pool or gym.
The Fear Factor: Breast Cancer Concerns
Beyond the realm of appearance-related anxieties lies another fear – the specter of breast cancer. Though statistically rare in men compared to women, having excess breast tissue can stoke fears about the potential risks of developing this disease.
However, it’s important to note that most cases are benign and do not directly increase one’s likelihood of developing breast cancer.
Mitigating Mental Health Impacts during Treatment
Effectively managing physical symptoms and mental health impacts requires more than just medical intervention—it also calls for robust emotional support systems. In addition to treatment options such as medication or surgery aimed at reducing glandular tissue size and restoring normal contouring around male breast areas, professional counseling may offer immense benefits.
- Emotional Support: Connecting patients with others who’ve faced similar experiences provides reassurance during difficult times—a sentiment echoed by countless other men who’ve successfully overcome their struggles through treatments like surgical procedures offered nationwide at SurgiSculpt clinics.
- Patient Education: Knowledge is power when dealing with gynecomastia—understanding you’re not alone can provide much-needed comfort while helping guide informed decisions about treatment plans.
As we delve deeper into understanding gynecomasty, let us focus on distinguishing between its types – glandular vs fatty variations along distinct stages ranging from I to IV.
Understanding Gynecomastia: Types and Stages
Gynecomastia is a complex condition that varies from person to person. To fully comprehend this medical issue, it is important to distinguish between the two primary types: glandular and fatty gynecomastia, each with distinct characteristics.
The Battle between Glandular and Fatty Gynecomastia
Glandular and fatty gynecomastia are like opposing chess players, each with its causes and physical features. Glandular gynecomastia is characterized by hormonal imbalances, resulting in the development of firm breast tissue beneath the nipple area. Fatty gynecomastia is typically connected to being overweight, where an abundance of fat stored in the chest area gives a breast-like appearance. It’s important to note that individuals can simultaneously exhibit elements of both types.
Exploring the Different Stages
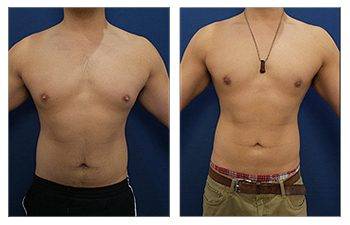
Aside from the types, gynecomastia is also classified into stages ranging from grade I to IV, based on the severity of the condition. Grade I is characterized by small enlargement without excess skin, while grade II involves moderate enlargement without extra skin.
Significant changes become evident as the condition progresses to more severe stages, such as grades III and IV. Grade III gynecomastia is marked by noticeable sagging due to increased skin presence and enlarged breasts. Grade IV takes feminization further by altering the diameter of the areola and repositioning the nipples to point downwards instead of outwards, as is typical in male chests.
The following section will examine how doctors diagnose grades I and II of gynecomastia through physical exams and patient history reviews. Stay tuned as we explore how doctors utilize physical examinations and patient history reviews to identify these specific forms of gynecomastia accurately. Learn more about this process here.
Unveiling the Diagnosis of Gynecomastia
A physical exam and medical history review are used to diagnose gynecomastia, a condition marked by an abnormal enlargement of male breast tissue. Your healthcare provider will delve deep into discussions about your symptoms and past health issues.
A key part of this conversation involves any significant weight changes you might have experienced. Rapid fluctuations can disrupt hormone levels, leading to gynecomastia. Another crucial aspect is reviewing any medications currently being taken since certain drugs, such as steroids or those for heart disease, could trigger this condition.
Your doctor’s physical exam would primarily focus on assessing the size and texture of your breasts. It is sometimes necessary to distinguish between true gynecomastia (growth of breast tissue) and pseudogynecomastia (fat deposition).
Diving Deep into Medical History Review
An extensive analysis of previous medical records helps pinpoint potential triggers like liver diseases or hormonal imbalances, which may contribute to breast enlargement. This includes examining whether there’s been a family history pointing towards a genetic predisposition for developing gynecomastia.
Navigating Physical Examination Techniques
Regarding hands-on inspection methods during diagnosis, palpation – feeling around the chest area for abnormal lumps – is a common practice among clinicians investigating suspected cases of gynecomastia.
Additional diagnostic tests, such as mammograms or ultrasounds, may be performed to delve deeper into suspicious findings from the initial evaluation. Blood tests are occasionally ordered to measure hormone levels to rule out other conditions causing enlarged breasts.
The combined approach when diagnosing gynecomastia uses personal health information and clinical examinations to identify possible underlying causes.
Once this condition has been successfully diagnosed based on its severity grading system ranging from Grade I (minor puffiness) to Grade IV (feminine-appearing breasts), we must consider suitable treatment options.
So, this naturally leads us to delve into the many ways you can handle different stages. This includes non-surgical methods like medication therapy and surgical interventions.
Understanding the Treatment Options for Different Gynecomastia Stages
Gynecomastia, characterized by enlarged breast tissue in males, has different stages, each requiring a specific treatment approach. Customizing the treatment to manage symptoms and address aesthetic concerns is essential.
Exploring Non-surgical Approaches to Managing Gynecomastia
In the early stages (Grade I & II) of gynecomastia, non-surgical treatments are often effective. Medications like anti-estrogens or aromatase inhibitors may be prescribed to even out hormonal changes, potentially leading to a decline in breast tissue.
A well-rounded lifestyle, regular exercise routines, and a balanced diet are also recommended. This helps regulate body weight, indirectly influencing estrogen levels. However, it’s important to note that the effectiveness of medication varies based on individual hormone profiles and the severity of the condition.
Considering Surgical Treatment Options for Gynecomastia
Surgical interventions may be necessary if non-invasive methods are unsuccessful or an individual has severe gynecomastia (Grade III & IV). The two main procedures available are liposuction surgery for gynecomastia and breast reduction surgery.
Liposuction surgery for gynecomastia aims to remove excess fat deposits around the chest area while preserving glandular tissues whenever possible. This less invasive method may not achieve the desired results in significant glandular hypertrophy or skin redundancy cases.
In contrast, breast reduction surgery is specifically designed for individuals with gynecomastia. It involves excisional techniques to remove surplus fatty tissues and extra glandular components, resulting in a flatter chest contour. This procedure is typically recommended for cases with significant sagging due to stretched skin envelopes, commonly found in Grade IV cases.
Learn how you can get rid of gynecomastia fast here.
As we delve deeper into this medical issue, we must remember that hormones, particularly testosterone versus estrogen, play a crucial role.
The Role of Hormonal Imbalance in Gynecomastia
Understanding the role of hormonal imbalance in gynecomastia begins with understanding how estrogen and testosterone interact. These two hormones, while commonly associated with their respective genders, exist within everyone’s body.
In men, testosterone typically takes center stage. High estrogen levels or low testosterone levels can cause gynecomastia, characterized by the enlargement of male breast tissue.
Hormonal Imbalance & Gynecomastia
A balanced ratio between these two hormones is crucial for maintaining typical male characteristics. But when this balance gets disrupted, things start going south. It could be due to certain health issues or lifestyle factors leading to increased estrogen production or decreased testosterone production.
This hormone upheaval often leads to gynecomastia, which presents itself across different stages – from slight enlargement without skin excess (Grade I) to marked enlargement with skin excess (Grade IV). Each stage brings its challenges and requires specific treatment approaches tailored according to individual needs and circumstances, including age and overall health status.
Role of Estrogen and Testosterone in Gynecomastia
Testosterone usually inhibits excessive fatty tissue development while promoting muscle mass gain. In contrast, despite being at lower levels than females, estrogen stimulates female characteristic traits such as breast growth among males. If either one experiences a disproportionate increase, it can result in abnormal developments like gynecomastia. Any imbalance of testosterone and estrogen can cause gynecomastia, thus necessitating a corrective intervention.
Medical interventions generally aim to restore these imbalances through medication or surgical procedures, depending on the severity of the case.
The complexities surrounding hormonal balances have now been discussed, allowing us to transition into exploring potential treatments, particularly in severe cases where non-surgical methods have proven ineffective, hence making surgery a necessary consideration.
Regarding Grade IV Gynecomastia, let’s dive deeper into this topic.
Surgical Intervention for Severe Cases (Grade IV)
Dealing with severe cases like Grade IV Gynecomastia can be challenging. However, understanding why surgical intervention is necessary and the processes involved simplifies things.
Let’s delve into what makes surgery an effective solution for these complex cases.
The Rationale Behind Surgical Treatment for Severe Cases (Grade IV)
You might wonder: Why opt for surgery for Grade IV Gynecomastia? Well, it boils down to two key reasons – excess glandular tissue and fat accumulation. These are aspects that non-surgical means often struggle to tackle effectively.
Gynecomastia Male Breast Surgery is typically recommended to restore natural male chest contours and remove this excess tissue. The procedure may involve liposuction or excision techniques depending on your specific condition.
Liposuction targets fatty deposits, while excision handles more complex issues such as sagging skin or enlarged areolas. Sometimes, both methods are used together – a strategy known as Combination Approaches for Severe Gynecomastias.
Digging Deeper Into Combination Approaches for Severe Gynecomastias
A combination approach leverages liposuction and excision techniques’ strengths, giving you optimal results from your treatment plan. So how does this work?
- Liposuction begins by making small incisions with a thin cannula inserted under local anesthesia to break up and suction out unwanted fat cells.
- In contrast, excision involves removing glandular breast tissues or excess skin directly using scalpel cuts when necessary. The decision between these two approaches depends heavily on whether there’s primarily fat (lipomastia) versus true gynecomastia tissue present.
Your health provider will help decide which method suits you best based not just on cosmetic outcomes but also physiological comfort—like alleviating tenderness or pain associated with severe gynecomastia—because, at the end of the day, restoring confidence alongside achieving physical relief is our ultimate goal.
Remember: Chatting with your doctor before making any health decisions is crucial.
FAQs about Gynecomastia Stages
What are the four stages of gynecomastia?
The four stages of gynecomastia include Grade I (minor enlargement, no skin excess), Grade II (moderate enlargement, no skin excess), Grade III (moderate enlargement with extra skin), and Grade IV (marked enlargement with extra skin).
What are the three stages of gynecomastia?
In some classifications, there are three main stages: mild or grade I (glandular tissue beneath the nipple-areola complex), moderate or grade II (enlarged breast tissue extending outside the nipple area), and severe or grade III (large breasts resembling female busts).
What does stage 1 gyno look like?
Stage 1 Gyno typically presents as small swelling around the nipples. It is usually barely noticeable and can often be mistaken for normal chest fat.
How fast does gynecomastia progress?
Growth rates vary from person to person, but pubertal onset generally peaks within six months to two years. Adult-onset progression depends on underlying causes such as hormonal imbalance or medication side effects.
Conclusion
Understanding the stages of gynecomastia is no longer a challenge. We have thoroughly explored this common male breast condition, highlighting its complexities. It is important to recognize that gynecomastia is not simply about tissue growth around the nipple area. It is a condition with different stages and types, each requiring unique intervention strategies.
The psychological impact of gynecomastia should not be ignored. It can sometimes lead to anxiety, psychosocial discomfort, and even a fear of breast cancer. From glandular to fatty gynecomastia, the symptoms can vary across different grades. Hormonal imbalance plays a crucial role in the development of this condition.
We have also discussed various diagnosis methods and highlighted the available treatment options for different stages of gynecomastia. Surgical intervention is often necessary in severe cases, such as Grade IV.
We at SurgiSculpt, your reliable choice for cosmetic plastic surgery, get it. We’re all about giving you care that’s customized to where you are in your gynecomastia journey. No need to let this condition slow you down! Swing by SurgiSculpt.com and see what we can do.