The Gynecomastia pinch test is a vital diagnostic tool in the medical world.
This simple procedure can provide crucial insights for those grappling with male breast enlargement. Using the gynecomastia pinch test, doctors can distinguish between glandular and fatty tissue to determine if it is gynecomastia or pseudogynecomastia, impacting treatment plans and surgical expectations. This distinction influences treatment options and potential surgical planning and recovery expectations. Navigating through the journey of gynecomastia can be overwhelming for many men. But understanding how tools like the Gynecomastia pinch test work can make all the difference.
Understanding Gynecomastia
Gynecomastia is a condition that can have a big impact on men of all ages, and it may be an emotionally trying experience. The main symptom is enlarged male breasts, which can be a source of embarrassment and self-consciousness.
The underlying cause of gynecomastia is often hormonal imbalances in the body. Weight gain can be a contributing factor to the development of gynecomastia, so it is important to consider this.
Distinguishing True Gynecomastia from Pseudogynecomastia
It is crucial to differentiate between true and pseudogynecomastia to identify and diagnose gynecomastia properly. While both conditions result in enlarged male breasts, their causes are different.
True gynecomastia occurs when breast tissue is overdeveloped due to hormonal imbalance. This is typically characterized by an excess estrogen or a testosterone deficiency, leading to epithelial tissue growth behind the nipple area.
On the other hand, pseudogynecomastia is not hormone-related. It occurs when excess fat accumulates around the chest region. Men with this condition have more adipose (fat) tissue than glandular tissue in their chests, making larger breasts appear.
Diagnosing Gynecomastia: The Pinch Test
Doctors use various methods, including physical examinations and imaging tests such as mammograms or ultrasounds, to accurately diagnose gynecomastia.
One specific diagnostic tool frequently used is the pinch test for gynecomastia. This test involves gently pinching the breast tissue to assess its composition. If the tissue feels firm or rubbery, it suggests the presence of glandular tissue, indicating true gynecomastia. On the other hand, if the tissue feels soft and fatty, it suggests pseudogynecomastia caused by excess fat accumulation.
The pinch test is crucial in determining the kind of gynecomastia someone has. This knowledge is vital for crafting the right treatment plan. It lets doctors make smart calls when it comes to surgery.
Demystifying the Gynecomastia Pinch Test
In diagnosing gynecomastia, which leads to the enlargement of male breast tissue, one cannot underestimate the value of a seemingly simple tool – the pinch test. This brief yet insightful examination is performed in-office and only takes a few fleeting moments.
A Closer Look at Conducting a Pinch Test
The process involves your healthcare provider using their thumb and forefinger to squeeze your breast tissue gently. The purpose? To differentiate between glandular and adipose (fat) tissue while identifying excesses. While it’s not painful, some patients might find it slightly uncomfortable.
Your journey with this procedure begins as you sit upright while your doctor pinches around your nipple-areola complex with their fingers. They’re on high alert for thickened areas, which could indicate abnormal growth or gynecomastia.
During this exploration, firm, rubbery lumps found beneath normal fatty tissues often signify excessive glandular tissues—a telltale sign of true gynecomastia—instead of pseudogynecomastia, where fat accumulation occurs without significant gland involvement.
Pivotal Role of Pinch Test in Surgical Planning
Treatment plans are tailored based on accurate diagnosis; understanding what causes breast enlargement can effectively guide surgical procedures. Herein lies the role of pinch test results—they reveal whether excess glandular tissue requires removal or if fat deposits primarily contribute towards increased chest size.
Surgical planning based on pinch test results provides doctors insights into how extensive surgery needs to be: If significant glandular overgrowth is detected via this method—more invasive approaches may become necessary compared to situations where adipose content predominates, which often require less aggressive techniques such as liposuction alone. Learn more about these conditions here.
Now that we’ve unveiled why “pinching” matters so much in treating gynecomastia let us explore other diagnostic tools used alongside it and how they collectively shape post-surgical outcomes.
Unveiling the Role of the Gynecomastia Pinch Test in Surgical Planning
The Gynecomastia pinch test is a powerful tool for diagnosing male breast enlargement. It allows surgeons to uncover excess glandular tissue, providing invaluable insight into the severity of the condition.
So, how does the pinch test work in conjunction with other diagnostic measures? Let’s delve deeper into its significance.

Merging the Gynecomastia Pinch Test with Other Diagnostic Measures
Combining the results of the pinch test with other diagnostic measures is critical to gaining a comprehensive understanding of gynecomastia. This amalgamation leads to more effective surgical planning and improved outcomes during the post-surgical phase.
First, discuss the importance of reviewing the patient’s medical history. Identifying any illnesses causing gynecomastia is essential, as the Mayo Clinic notes hormonal imbalances or certain medications may be contributing factors. The Mayo Clinic, one of our trusted sources, highlights the role of hormonal imbalances or certain medications as potential culprits behind this condition.
In addition to physical examinations like the pinch test, imaging techniques such as mammograms or ultrasounds also play a significant role when necessary. These imaging techniques provide a comprehensive assessment of each patient’s case. A study by the NCBI emphasizes how thorough preoperative evaluations contribute to the success of breast reduction surgeries for men.
With your newfound understanding of gynecomastia and the diagnostic significance of the pinch test, among other measures, you are now equipped to explore the various surgical options available. These options can be tailored to individual cases, ensuring optimal outcomes and patient satisfaction.
Effective Treatments for Gynecomastia
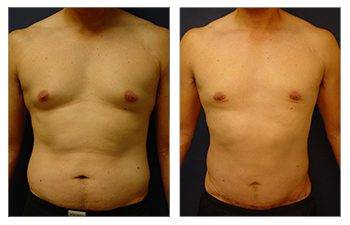
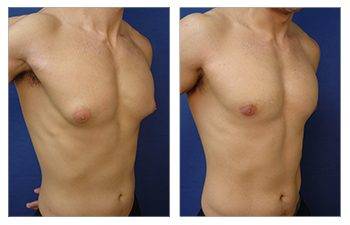
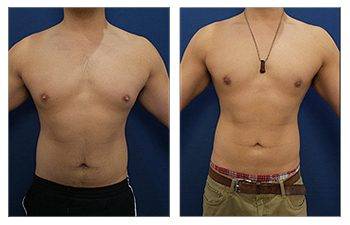
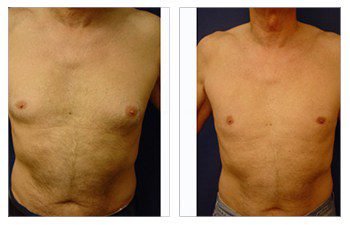
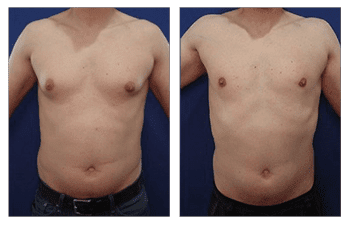
The realm of cosmetic plastic surgery can present a selection of remedies for gynecomastia, an affliction denoting the expansion of male breast tissue. Depending on individual cases, treatment options can vary from liposuction to surgical removal of glandular breast tissues.
Liposuction: A Solution for Excess Fat
How does one address the excess fat and skin associated with gynecomastia? The answer lies in liposuction. This procedure not only reduces volume but also contours the chest area. It is particularly effective when fatty tissue is more prevalent than glandular tissue.
But what if there are substantial amounts of dense, firm glandular tissues that liposuction alone cannot eliminate?
Surgical Removal: Addressing Glandular Breast Tissues
In such cases, surgeons may recommend a more comprehensive intervention – direct excision or surgical removal of these enlarged glands. Combining this method with liposuction often leads to optimal results in breast reduction surgery for men dealing with excessive fat and enlarged glands.
- Liposuction could be your best option if you primarily have excessive fat deposits rather than enlarged glands.
- A combination therapy involving both methods might provide optimal results if you have both conditions (excessive fat and enlarged glands).
- Ideal candidates for surgery are fully grown individuals who maintain a healthy body mass index without any notable hormonal imbalance or illnesses contributing to their condition.
In addition to reducing volume through techniques like liposuction, addressing sagging skin due to weight loss or aging is also an integral part of the process.
Now that we have explored how physical manifestations can be addressed surgically let’s delve deeper into another equally crucial aspect – the emotional well-being post-surgery.
Next, we’re diving into “Dealing with the Emotional Rollercoaster of Gynecomastia.” We’ll uncover strategies to keep your spirits high throughout this journey.
Navigating the Emotional Landscape Post-Gynecomastia Surgery
Addressing gynecomastia is not just about physical changes. Exploring this altered landscape can deeply impact one’s mental health, emotional state, and interpersonal relationships. But how do you navigate this new terrain? The American Academy of Family Physicians offers some insight.
“Embracing one’s body post-surgery requires time and patience, but with appropriate coping strategies and promoting positive mental health practices, it becomes easier.”
Fostering a positive body image after surgery for treating gynecomastia is crucial – an essential step toward overall recovery.
Cultivating Positivity After Gynecomastia Treatment
The aftermath of surgical treatment isn’t just about healing physically; there are emotional scars to heal, too. Here are a few effective approaches:
- Acknowledge your feelings: Recognize your emotions regarding your changed appearance.
- Talk openly: Conversations with loved ones or support groups can provide reassurance during these times.
- Promote Mental Wellness: Techniques such as meditation or yoga could help manage stress levels post-surgery.
Finding Support In Your Journey Towards Positive Body Image
Mental Health Resources: Consider seeking professional help if dealing with residual anxiety or distress related to the change in physique seems overwhelming.
Support Networks: If you’re feeling alone on this journey, remember there are online forums like Gynecomastia.org Forum. This platform allows individuals who have undergone similar experiences to share their stories, providing comfort and camaraderie.
Your Unique Recovery Pathway: Embrace Change With Patience
I’m sorry, but your request is incomplete. Could you please provide the last paragraph that needs to be rewritten? This will help me give a more accurate response.
Embarking on the Recovery Journey After Surgery
Navigating the recovery phase after surgery, especially in cases of gynecomastia, is a crucial part of your journey to wellness. This involves physical healing and effectively managing pain and discomfort for successful long-term outcomes.
1. Mastering Pain Management: Your Key to a Comfortable Recovery
Pain management post-surgery is not simply about taking pills at regular intervals; it requires understanding and patience. It is essential to adhere to prescribed medications and avoid using over-the-counter drugs without consulting your surgeon.
In addition to medication, there are other options you can explore, such as gentle exercises that studies show can help reduce swelling and prevent blood clots by improving circulation. Research supports the benefits of these exercises.
2. Handling Discomfort: Embracing Changes & Moving Forward
Surgical procedures bring about physical changes that may cause emotional distress or anxiety due to temporary limitations on daily activities or altered body image. Remind yourself that these changes are a part of the recovery journey, and you’re not alone in this.
You may find comfort in calming methods like taking slow, deep breaths or meditating. Research suggests that these practices significantly reduce stress levels following surgical procedures. Additionally, mental health support is vital in achieving optimal long-term outcomes from your procedure.
3. Recovery Timeline: Setting Realistic Expectations?
The road to normalcy varies based on individual factors, including age, general health status, and the type of procedure undergone. Generally, it takes a few weeks to resume normal day-to-day activities following cosmetic plastic surgery. If complications arise, do not hesitate to consult with your healthcare provider for necessary guidance.
- Avoid strenuous activity until the doctor advises: Overexertion can lead to complications and slow the overall healing time.
FAQs about Gynecomastia Pinch Test
How to Test Yourself for Gynecomastia
You can perform a simple self-exam by feeling your chest area. If there is a firm, rubbery mass beneath the nipple and areola region, it could be indicative of gynecomastia.
How to Determine if You Have Gynecomastia or Just Fat
The key difference lies in the texture. Gynecomastia presents as glandular tissue, which feels firmer than fatty tissue. It is recommended to seek a professional diagnosis through a pinch test or imaging for accurate differentiation.
What Does a Gynecomastia Lump Feel Like?
A typical gynecomastia lump feels like a small disk-shaped mass of firm tissue directly under the nipple-areolar complex that moves synchronously with skin movement.
Does Gynecomastia Cause Pain When Pressed?
Glandular breast tissues associated with true gynecomastia may cause tenderness or pain upon pressing, while pseudogynecomastia usually does not cause discomfort.
Conclusion
- Unraveling the mysteries of gynecomastia can be a daunting task.
- The condition, often distressing and confusing for many men, has solutions.
- Enter the Gynecomastia pinch test – your ticket to clarity.
- This simple diagnostic tool differentiates between glandular tissue and adipose tissue. Identifying true gynecomastia or pseudogynecomastia is imperative for determining the best treatment course and expectations of surgical planning.
- Your treatment options hinge on this crucial distinction. So do surgical planning and recovery expectations!
- Gynecomastia isn’t just about physical discomfort; it takes an emotional toll. However, effective coping strategies are available to help manage its impact on mental health.
- Surgery is not always the answer, but when necessary, know that various procedures effectively cater to individual cases. From liposuction to removing glandular breast tissues – each option is designed with patient safety and long-term results in mind.
The journey doesn’t end at surgery, though! The road to recovery might seem challenging initially, but remember: proper care leads to successful outcomes.
Ready for change? Let us guide you through every step, from diagnosis to post-surgical care.