Introduction: Complication Statistics for Liposuction in 2024
In 2024, the overall risk of serious complications following liposuction lies at 2.4%. When liposuction is combined with supplemental ancillary procedures, then the complications may rise to 3.5%. Based on current literature, major complications of liposuction include infection (0.1-6.8%), seroma (0.1-14.2%), hematoma (0.3-4.7%), skin necrosis (0.2-0.5%), and pulmonary complications such as fat embolism (0.01-0.03%) and pulmonary edema (0.01-0.3%).
The overall low incidence of complications in recent liposuction procedures can be attributed to advancements in techniques, improved patient selection, and surgeon expertise. Specifically, the use of the tumescent technique, smaller cannulas, and better patient monitoring have contributed to the reduced risk of complications.
Liposuction continues to be a popular cosmetic procedure in 2024, with advancements in technology and techniques leading to improved results and safety. As with any surgical procedure, it is important to keep track of complication statistics to ensure the continued safety and effectiveness of liposuction. In this article, we will explore the latest complication statistics for liposuction that will extend into 2024, shedding light on the most common issues that can arise, as well as the steps being taken to minimize these risks and improve patient outcomes.
Understanding the current landscape of liposuction complications is crucial for both surgeons and patients and can help to inform decision-making and promote responsible and informed choices regarding this widely sought-after cosmetic procedure.
Hypothermia
Hypothermia can lead to various complications, including impaired coagulation and immune system function. Prolonged exposure to cold temperatures can cause vasoconstriction, leading to reduced blood flow to the extremities and vital organs, increasing the risk of blood clot formation and impaired blood clotting. Furthermore, hypothermia can suppress the immune response, making individuals more susceptible to infections.
To prevent excessive heat loss and mitigate the risk of hypothermia, it is essential to use warming devices such as blankets, heating pads, or heated air blankets. Additionally, providing warm fluids and maintaining a comfortable room temperature can help prevent hypothermia. It is crucial to dress in layers, keep dry, and seek shelter in a warm environment when exposed to cold weather.
In conclusion, hypothermia can have significant impacts on coagulation and immune systems, but by taking basic preventive measures such as using warming devices, consuming warm fluids, and paying attention to room temperature, the risk of hypothermia can be reduced.
Lidocaine and epinephrine toxicity
Lidocaine and epinephrine are commonly used in liposuction procedures, but they can have potentially toxic effects if not used carefully. The accepted dose of lidocaine is up to 35 mg/kg, with a peak concentration of 7-10 mcg/mL. Epinephrine is typically used at a concentration of 1:100,000 to 1:1,000,000. It is essential to consider factors such as liver metabolism and cardiac function when using these drugs in liposuction.
Overdosing on lidocaine can lead to symptoms such as dizziness, drowsiness, seizures, and even cardiac arrest. Epinephrine, on the other hand, can cause hypertension, arrhythmias, and angina, especially in patients with underlying cardiac conditions. Contraindications for using epinephrine include uncontrolled hypertension, hyperthyroidism, and certain medications that interact with epinephrine.
To address potential toxicity, it is crucial to carefully calculate the doses of lidocaine and epinephrine based on the patient’s body weight and adhere to the recommended maximum doses. Additionally, pre-existing cardiac conditions should be thoroughly evaluated before using epinephrine, and close monitoring of the patient’s vital signs during the procedure is necessary.
In case of toxicity, prompt intervention and administration of antidotes or supportive measures should be initiated. Overall, a thorough understanding of the potential toxicity of lidocaine and epinephrine, along with close attention to patient-specific factors, is crucial for ensuring the safety of liposuction procedures.
Cardiopulmonary arrest & fluid shifts
Pre-operative fluid management should focus on optimizing perfusion without causing excessive fluid shifts. Patients should be adequately hydrated but with limitations on fluid aspirations to avoid third spacing. Fluid aspirations should be limited to 5 L per session and less than 5% of the patient’s body weight. Intra-operatively, careful monitoring of fluid balance is essential to prevent excessive increases or decreases in fluid volume, which can impact cardiopulmonary function. It is important to treat less than 30% of the body surface to minimize fluid shifts, which can affect perfusion and lead to cardiopulmonary complications.
Post-operative fluid management should aim to maintain adequate perfusion while avoiding over-hydration or dehydration. Monitoring for signs of third spacing and adjusting fluid therapy accordingly is crucial to avoid complications. Attention should be paid to the patient’s cardiovascular and respiratory status to ensure that fluid management is not contributing to cardiopulmonary issues.
Wound Infection
Common signs and symptoms of wound infection after plastic surgery include redness, swelling, warmth, and pus at the surgical site. Other indicators of infection may include increased pain or tenderness, fever, and a foul odor coming from the wound. In severe cases, the patient may require IV antibiotics to address the infection.
Proper wound care after plastic surgery is essential to prevent infection. This includes keeping the wound clean and dry, changing the dressings as instructed, and avoiding getting the wound wet. It is also important to follow post-operative care instructions provided by the surgeon or healthcare provider. If any signs of infection are present, such as increased pain, redness, swelling, or pus, it is crucial to seek medical attention promptly.
In summary, staying vigilant for signs of infection and seeking prompt medical attention if any concerning symptoms arise is essential for proper wound care after plastic surgery. This can help to ensure the best possible outcome and reduce the risk of complications.
Fat emboli
Fat emboli syndrome is a rare condition that occurs when fat particles enter the bloodstream and block blood vessels. It most commonly happens as a complication of long bone fractures, especially in the lower extremities. The classic triad of symptoms includes a petechial rash, respiratory distress, and cerebral dysfunction. The petechial rash is often seen on the chest and conjunctiva and is a result of small blood vessel leakage. Respiratory distress can range from mild to severe and may progress to acute respiratory distress syndrome (ARDS). Cerebral dysfunction can include confusion, disorientation, and even coma.
Diagnosing fat emboli syndrome can be difficult, as the symptoms can be nonspecific and may mimic other conditions. Imaging studies like chest X-rays, CT scans, and MRI can help identify fat emboli in the lungs or brain. Treatment is largely supportive, with a focus on managing symptoms and providing respiratory support if necessary.
Corticosteroids have been proposed as a potential treatment for fat emboli syndrome, as they can help reduce inflammation and stabilize cell membranes. However, their role in managing this condition is still not well-established, and further research is needed to determine their efficacy.
Overall, fat emboli syndrome is a rare but serious complication of long bone fractures, and early recognition and supportive care are crucial in managing this condition.
Perforation of abdomen and viscera
Perforation of the abdomen and viscera during suction lipectomy can be caused by various factors, including the lack of proper training in the technique, the use of power-assisted cannulas that can increase the risk of accidental puncture, and improper patient positioning during the procedure. Using sharp cannulas instead of blunt ones can also increase the risk of perforation, as they can more easily penetrate deeper than intended.
It is crucial to use blunt cannulas during suction lipectomy to minimize the risk of puncturing important structures within the abdomen and viscera. Sharp cannulas can lead to unintended damage to internal organs, blood vessels, or nerves, which can result in serious complications for the patient.
To prevent these complications, it is important for the surgeon to have a thorough understanding of anatomical structures and to have extensive experience in handling soft tissues. Additionally, careful use of power-assisted technologies and maintaining proper patient positioning are essential to minimize the risk of perforation during suction lipectomy.
In summary, avoiding using sharp cannulas, ensuring proper training and experience, and employing careful techniques are crucial to preventing perforation of the abdomen and viscera during suction lipectomy.
Hemotomas and Seromas
Local complications that can occur after liposuction include hematoma, which is a collection of blood under the skin, and seroma, which is a collection of fluid. Additionally, contour deformities and skin irregularities can also occur, leading to uneven or bumpy skin texture.
Risk factors for these complications include excessive liposuction, poor surgical technique, and patient-related factors such as age, smoking, and certain medications. The recommended management and treatment options for these complications include drainage of the hematoma or seroma, massage therapy, and in some cases, revision liposuction to correct contour deformities.
The incidence and prevalence of these complications vary among different patient populations and surgical techniques. Patients with preexisting medical conditions or those who undergo large-volume liposuction are at higher risk for developing these complications. Additionally, the use of ultrasound or laser-assisted liposuction may also increase the risk of complications.
In conclusion, understanding the local complications of liposuction and their associated risk factors is crucial for both patients and clinicians to minimize the occurrence of these complications and ensure successful outcomes.
Skin Compromise
Skin compromise may occur if blood flow becomes blocked to focal areas of the skin. Vascular compromise is a theoretical possibility when we consider that liposuction utilizes rods that may mechanically irritate the blood vessels. The criteria that must be followed to avoid vascular skin compromise follow the premise of angiosomes. Angiosomes describe palm-sized areas of the skin which map out the entire body in 100 palm-numbered areas. Each angiosome is supplied by its direct blood flow.
Preservation of vascularity includes the principle that any angiosome of skin can have its vascularity preserved even if its blood direct blood vessels are compromised by an adjacent angiosome that is not compromised. This angiosome preservation concept describes the principle that as long as a single adjacent angiosome is preserved next to an angiosome that has its vascular supply compromised, that angiosome will survive. This concept must be utilized during liposuction to minimize the risk of blood flow to the skin.
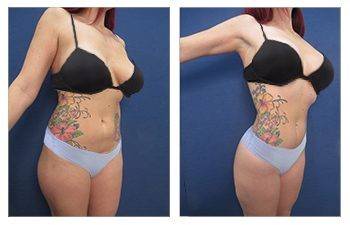
Contour Irregularities
Contour irregularities in liposuction procedures can be caused by a variety of factors, including inadequate tissue assessment, improper cannula orientation, and suboptimal postoperative care. Proper technique is crucial in reducing the risk of contour deformity. This approach emphasizes the importance of assessing the quality of the tissues and using a three-step process to emulsify the fat before suctioning it out, resulting in smoother and more even results.
Postoperative dressings also play a key role in ensuring proper healing and minimizing the risk of contour irregularities. Compression garments can help maintain the new shape of the treated area and reduce swelling while minimizing the risk of uneven fat distribution.
Treating preexisting cellulite deformities can be challenging, but the use of autologous tissue interposition, where the patient’s own fat is used to fill in the irregularities, can help improve the overall contour of the treated area.
Ultimately, the prevention of contour irregularities in liposuction procedures requires a combination of proper technique, meticulous tissue assessment, and attentive postoperative care.
Is Liposuction Safe?
Liposuction is generally considered safe, but it’s important to take certain precautions to ensure a successful procedure. Before undergoing liposuction, it is crucial to discuss your medical history with your cosmetic surgeon to determine if you are a suitable candidate for the procedure. It is also important to avoid certain medications and supplements that can increase the risk of bleeding and other complications.
In the weeks leading up to your liposuction procedure, it is advisable to complete physically tasking jobs and activities to reduce the risk of injury and promote healing. Additionally, maintaining a healthy weight and exercise regimen can improve the overall outcome of the procedure and reduce the risk of complications.
Following the liposuction procedure, it is essential to adhere to the post-op instructions provided by your surgeon. This may include wearing compression garments, taking prescribed medications, and avoiding strenuous activities. By following these safety precautions and considerations, you can minimize the potential risks associated with liposuction and achieve optimal results.
Frequently Asked Questions regarding Liposuction Complications
Liposuction is a popular cosmetic procedure that aims to remove excess fat from various parts of the body. While it is generally considered safe, like any surgical procedure, it comes with potential complications. In this article, we will address some frequently asked questions about liposuction complications. From the risks and side effects to ways to minimize the chances of complications, we will provide valuable information for anyone considering or undergoing this procedure. Understanding the potential drawbacks and how to mitigate them is essential for anyone considering liposuction, and we aim to provide clear and concise answers to common concerns regarding complications.
What are the risks of liposuction surgery?
Potential risks and complications associated with liposuction surgery include infection, embolism, inflammation, nerve damage, and fatality. Infection can occur at the incision sites and may require antibiotics or additional medical treatment. Embolism, the blockage of a blood vessel by a clot or other matter, can lead to serious complications such as organ damage or even death. Inflammation and swelling are common after the procedure and may persist for several weeks. Nerve damage can result in numbness, tingling, or changes in sensation in the treated area.
Statistics on the risk of death from liposuction vary, but studies have reported a mortality rate of approximately 20 in 100,000 liposuction procedures. Common risks such as infection and inflammation are usually managed with proper post-operative care, while rare but serious complications like embolism and fatality highlight the importance of selecting a qualified and experienced surgeon and closely monitoring for any adverse reactions during and after the procedure. Overall, it is crucial for patients to fully understand the potential risks and complications associated with liposuction surgery before making a decision.
How much blood loss occurs with liposuction?
Tumescent liposuction, which involves the injection of large amounts of a dilute solution containing lidocaine and epinephrine, typically results in minimal blood loss. The epinephrine helps to constrict blood vessels, reducing bleeding during the procedure. Additionally, the use of local anesthesia in tumescent liposuction further minimizes the risk of blood loss compared to general anesthesia.
The “safe” amount of fat to remove during liposuction is often determined by the patient’s body mass index (BMI). Higher BMI levels are associated with a higher risk of complications, including excessive blood loss. As a general guideline, no more than 5 liters of fat should be removed during a single liposuction session, with larger volumes associated with a greater risk of complications.
Factors that may lead to excessive blood loss after liposuction include the use of certain medications, such as blood thinners, and the volume of tissue removed. Patients with pre-existing medical conditions or those taking medications that affect bleeding should inform their physician to minimize the risk of excessive blood loss during liposuction.
What is the risk of infection with tumescent liposuction?
The risk of infection with tumescent liposuction is generally very low. Serious infections following liposuction surgery are rare, but they can occur. However, the use of the Tumescent Technique, which involves the infusion of a large volume of dilute lidocaine and epinephrine into the fatty tissue, actually helps to minimize the risk of infection.
Lidocaine, a common local anesthetic used in the Tumescent Technique, has bactericidal properties that can help reduce the risk of infection. This is because lidocaine can kill certain types of bacteria, helping to keep the surgical site free from infection. Additionally, the use of sterile technique, antibiotics, and proper wound care further minimizes the risk of infection when performing tumescent liposuction.
Overall, while there is always a risk of infection with any surgical procedure, the Tumescent Technique, along with proper sterilization and wound care, helps to greatly minimize the risk of infection with tumescent liposuction.
What major complications have been associated with liposuction?
Major complications associated with liposuction include pulmonary thromboembolism, which can occur when a blood clot travels to the lungs and blocks the blood flow; infection at the surgical site, which can lead to severe complications if not promptly treated; intra-abdominal perforation with visceral injury, where the abdominal wall or organs may be accidentally punctured during the procedure; hematoma or seroma, which are collections of blood or fluid under the skin that can cause discomfort and require drainage; nerve damage, which can lead to numbness, tingling, or muscle weakness in the treated area.
Other complications can include swelling or edema, which can be prolonged and affect the final result of the procedure; skin necrosis, a rare but serious complication where the skin tissue dies; pulmonary edema, a buildup of fluid in the lungs that can be life-threatening; adverse drug reactions to anesthesia or medications used during the procedure; and in rare cases, death.
These complications highlight the importance of carefully considering the risks and benefits of liposuction and selecting a qualified and experienced surgeon to perform the procedure.
Conclusion: Complication Stats for Liposuction in 2024
This blog highlights the importance of proper patient assessment, intraoperative monitoring, and early recognition of potential complications during liposuction procedures. By staying vigilant and adhering to best practices, surgeons can continue to minimize the risk of complications and ensure patient safety during liposuction.